 NHS England's Genomics Unit commissioned a 2-year Nursing and Midwifery Transformation Programme, led by Dr. Naomi Chapman and Dr. Emma Tonkin, with the aim of exploring nursing and midwifery inputs across seven cancer or rare disease clinical pathways, to broaden genomic knowledge and skills within NHS mainstream care, and improve quality of outcomes and experience for patients and their families.
NHS England's Genomics Unit commissioned a 2-year Nursing and Midwifery Transformation Programme, led by Dr. Naomi Chapman and Dr. Emma Tonkin, with the aim of exploring nursing and midwifery inputs across seven cancer or rare disease clinical pathways, to broaden genomic knowledge and skills within NHS mainstream care, and improve quality of outcomes and experience for patients and their families.
The North West Genomic Medicine Service Alliance led the National Lung Cancer Pathway Genomics Project, using a national approach that involved the remaining six regional GMSAs.
Each GMSA identified and invited clinically engaged subject matter expert Lung Cancer Nurse Specialists (LCNS), to participate in a scoping exercise and a series of five workshops.
The project team undertook an initial scoping exercise with the Lead Lung Cancer Nurse for Greater Manchester Optimal Lung Cancer Pathway; this pathway exemplifies best practices for this project.
Initially, a process mapping exercise based on the 'stepping stones' of a patient journey provided an overview on which to explore LCNS opportunities to address genomics with patients and their families.
The LCNS identified vital points across the patient pathway, where genomics featured and can be embedded to increase equity of access and reduce variation. Sharing insights into genomics in practice helped evaluate the knowledge, skills, and competency requirements needed to embed genomic medicine and facilitate genomic testing.
In the UK, lung cancer remains the most common cause of cancer-related death and is responsible for 35,000 deaths per year in the UK alone (Royal College of Physicians 2022) Genomic pathology results determine how lung cancer is treated both in the first-line setting and subsequent progression. The need to reach a diagnosis as soon as possible to improve patient outcomes of both survival and symptom burden/ quality of life for those living with lung cancer is imperative (Beckett et al. 2022).
‘Non-smoking associated lung cancer,’ (alternatively named Oncogenic Mutation Driven Lung Cancer - OMDLC) is a different disease entity from both an epidemiological and biological view (Peddireddy 2016, Planchard et al. 2018) and occurs in around 10-20% of patients with Non-small cell lung cancer (NSCLC). Delays in treatment commencement for those with an OMDLC have been proven to cause multiple adverse events including patient progression, hospitalization, and overall survival (Blanc–Durand et al. 2021).
Around Times (TATs) for lung cancer biopsies are highly variable and pathways can be confusing to both patients and clinicians (Royal College of Physicians 2020). The National Optimal Lung Cancer Pathway (NOLCP) target to reduce the time from first presentation to commencement of an anticancer treatment to 49 days (previously 62) is a challenging one and demands a review into service investment within all related diagnostic and treatment services including pathology (NHSE 2020, Royal College of Physicians 202 & 2020)
Drawing on the national optimal lung cancer pathway (NOLCP) published in 2017 and updated in 2020, the guidance 'Faster Diagnostic Pathways: Implementing a Time Lung Cancer Diagnostic Pathway (2022)' sets our guidance to achieve lung cancer diagnosis within 28 days from the first presentation of symptoms (pre-diagnosis).
The Greater Manchester Optimal Lung Cancer Pathway was developed and tested as a variation on the NOLCP. Optimising all pathway processes, Manchester University Hospitals NHS Foundation Trust Lung Cancer Service is recognised for achieving minimum waiting times, through service improvement and redesign.
The faster diagnostic pathway guidance recommends that all confirmed cancer tumour tissue samples are tested for all molecular markers (genomic tests) to determine patient treatment plans and management.
The Lung Cancer Pathway Genomics Project is one of seven projects within the two year NHS England Genomics Unit commissioned Nursing and Midwifery Genomic Transformation Progamme.
The Programme aims to explore nursing and midwifery inputs to clinical pathways, to broaden genomic knowledge and skills within NHS mainstream care, to improve outcomes and experience for patients and families.
Project outputs include:
- The Lung Cancer Clinical Pathway Initiative
- Equity of Access
- GeNotes
- Infographics
- Patient story
Workshop focus groups led to the LNCS identifying four distinct lung cancer pathway stages:
- Pre-diagnosis
- Cancer diagnosis
- Molecular diagnostics
- Post diagnosis
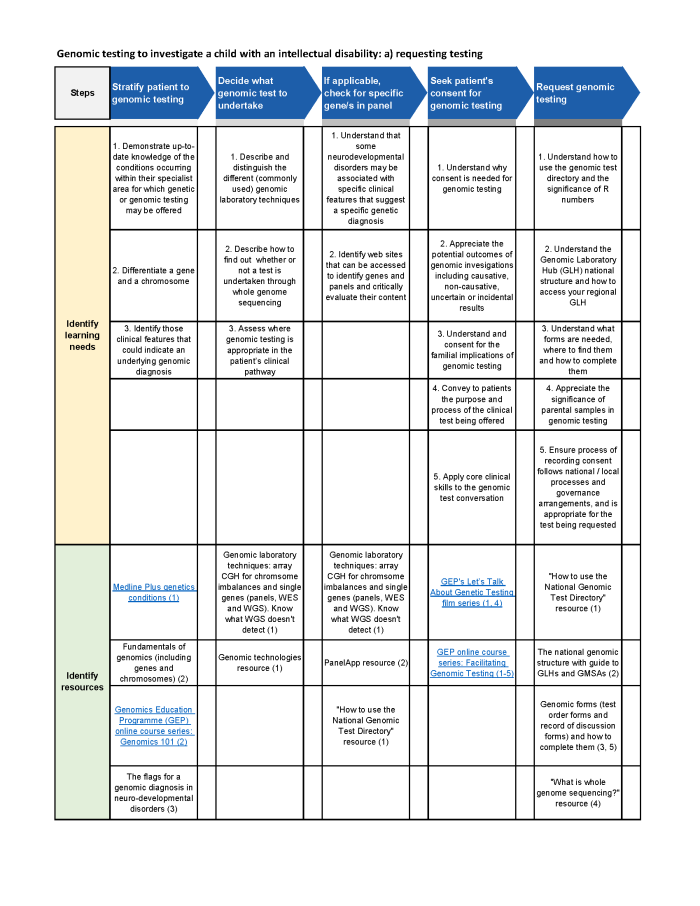
Utilising these insights the project team applied the stages to the steps within the Health Education England Clinical Pathway Initiative for Lung Cancer, enabling identifiable learning needs, corresponding teaching, learning, and educational resources.
The full Lung Cancer Pathway Initiative document can be viewed here.
Further insights from the LCNS illustrated differing levels of knowledge and skill would be required. Influenced by Benner's classification system, four levels were developed building up from a fundamental foundation level genomic novice, to genomic competent, genomic proficient, and genomic expert levels for those nurses wishing to develop advanced knowledge and skills.
 The Lung Cancer Pathway Genomics Project explored the activities needed to build an evidence base of best practice, to support the use of genomics across lung cancer services.
The Lung Cancer Pathway Genomics Project explored the activities needed to build an evidence base of best practice, to support the use of genomics across lung cancer services.
Producing a national picture that describes a 'gold standard' of how nurses can bring genomics into the lung cancer pathway.
The project identifies competencies and training needed to deliver this and facilitate adoption and sperad of genomic literacy, across lung cancer nursing.
An infographi is available to signpost healthcare professionals to education and training support. Available to view and download here: Genomics and You: Complete Me Infographic.
Genomic Novice resources are aimed at nurses and healthcare professionals requiring a foundation level of Genomics knowledge. (Fundamental)
This is the first of four levels of self-directed learning, developed as part of the National Nursing and Midwifery Genomic Transformation Programme - Lung Cancer Pathway Genomics Project.
The curated collection of resources includes signposting to NMC’s Regulatory Standards indicating the need for all registered nurses to understand Genomics.
HEE Genomics Education Programme modules outline the skills and knowledge required to prepare our workforce professionals to harness the potential for genomic medicine.
Cancer Research UK and Macmillan produce resources in an easily accessible format using animation to explain Lung Cancer and can be offered to patients and families for support.
- Cancer Research UK Understanding cancer genomics (1)
- Cancer Research UK - YouTube - What is lung cancer (6)
- Macmillan Cancer Support - Lung Cancer (6)
Links to crucial national Lung Cancer Guidelines aim to give an overview of current clinical developments and standards for care and links to professional organisations specific to Lung Cancer Nurses and the Professional Development Framework for Lung Cancer Nurse Specialists.
- National Optimal Lung Cancer Pathway (NOLCP) (1)
- Lung Cancer Nurses UK (1)
- NICE guidelines for lung cancer (2)
- LCNUK Professional Framework FINAL.pdf
Practical resources to support genomic medicine in Lung Cancer clinical settings are provided via HEE GEP GeNotes and links to the NHSE National Cancer Genomic Test Directory.
Genomic Competent resources build on the Novice level and includes a New Competency Framework for Genomic Testing. (Competency)
- NHS England Accelerating genomic medicine in the NHS A strategy for embedding genomics in the NHS over the next 5 years. (4)
- Human Tissue Act 2004 (3)
- ctDNA_ Examining liquid biopsy in cancer management (4)
- Genomics in Nursing - Genomics Education Programme (hee.nhs.uk)
- New competency framework for genomic testing - Genomics Education Programme (hee.nhs.uk)
- ctDNA Testing Pilot Programme (4)
- Joint Committee on Genomics in Medicine: Consent and confidentiality in genomic medicine (4)
- PHG Foundation; 'The GDPR and genomic data' (4)
- GEP online course: Facilitating Genomic Testing - Data and Sample Management in the NHS GMS (30 mins) (4
- GEP's Let’s Talk About Genetic Testing film series eg. Let’s Talk About… Communication Strategies (2,5)
- Dr Jargon: Genomics (5)
- Genomics Conversation: An Introduction to the week with Dr Anneke Seller NHS Genomic Medicine Service
Genomic Proficient resources introduce the nurse to an enhanced level of practice capable of independent practice and include the Competency Framework for Facilitating Genomic Testing. (Enhanced - CPPD modules)
- The Genomics Era: the Future of Genetics in Medicine (Future Learn MOOC)
- Molecular Pathology of Cancer and Application in Diagnosis, Screening and Treatment (CPPD module, blended learning, up to 6 weeks) (1,2,3,4)
- Introduction to the Counselling Skills used in Genomic Medicine (CPPD module, blended learning, up to 6 weeks) (2)
Genomic Expert is aimed at nurses wishing to advance their knowledge and skills through master’s level education to evaluate the impact of genomics within the clinical pathway and explore equity of access. (Advanced - Masters level).