Genomics is the study of an organism's entire genetic makeup, including its DNA sequence and the interactions between genes. But how does genomics relate to public health?
The information ‘stored’ within our genes can provide valuable insights into our predisposition to certain diseases, our responses to medications, and even our susceptibility to environmental factors, known as epigenetics. This knowledge has immense potential to transform how we approach public health initiatives.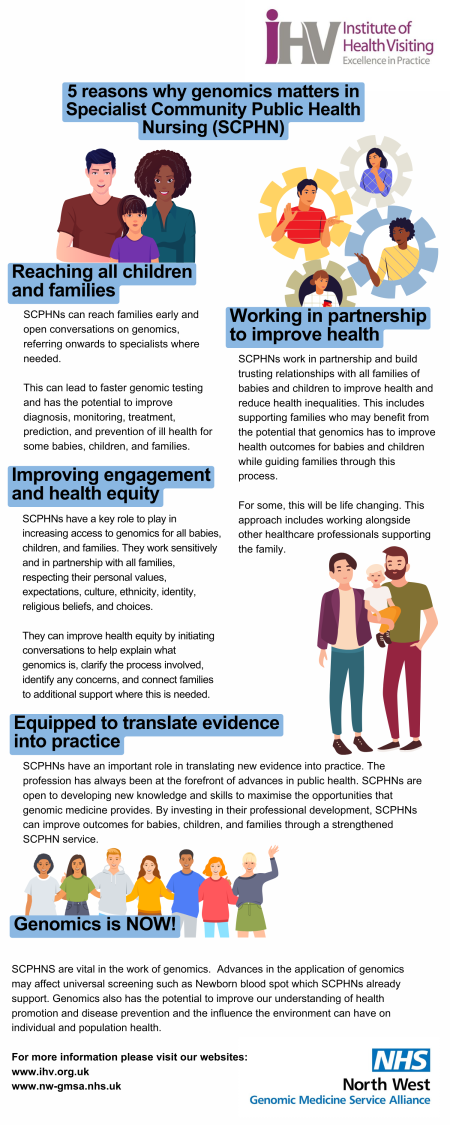
Genomics can enhance our understanding of how an individual’s genetic makeup affects their response to medications. Pharmacogenomics has the potential to revolutionise medication prescriptions, ensuring that patients receive the right medication, in the right dosage, as well as minimizing adverse effects and enhancing treatment outcomes.
One of the most significant contributions of genomics to public health is in the realm of disease prevention.
By analysing an individual's genetic profile, the presence of certain genetic changes or mutations, that increase the risk of specific diseases can be identified. Imagine being able to tailor or personalise healthcare, and health recommendations based on a pre-determined genetic makeup and identified ‘risk’ of developing certain cancers or disease, before they manifest themselves?
Institute of Health Visiting
We have recently collaborated with the national Institute of Health Visiting, on a new infographic (shown and available to download here), as well as hosting a Genomics Ambassador event for over 40 health visiting teams, across the North West.
We regularly hold webinars via Microsoft Teams, so we'd value your feedback on any future events and topics that you would like to see covered. To share your thoughts, please click here to complete our quick 60 second survey.
Within the webinar, Dr Saghira Malik Sharif, referenced her published paper 'Enhancing inclusion of diverse populations in genomics' PDF, which is avaialble to view here.
Health visitors hold a very special, trusted relationship with the families that they serve, so having the opportunity to discuss genomics as appropriate, confidently and competently, via active listening and non-verbal cues, supports their practice and ultimately enhances the care they provide.
Regarding cultural competencies, when identifying child development milestones – physical, cognitive and emotional, and where parental concern has been raised, red flags, or potential developmental delays highlighted, this should be discussed with parents, avoiding undue stress which is difficult when an emotive subject.
Being able to refer the child for genomic, or genetic testing enables the signposting of the child and their family to a potential diagnosis for childhood or rare disorders, or identification of a previously undiagnosed inherited risk. Again, cultural competency is paramount.
Having an understanding or knowledge of the perspectives of different populations regarding genomics is crucial, both to understanding the potential genetic variations among diverse ethnic groups, and providing culturally competent care.
Health visitors hold many relationships, many of which are cross agency i.e. Police, Social Services, Education, so maintaining those networks is fundamental to the care and support they provide to our families.
Typically, a health visitor is the first to identify where a child may have an rare disease or undiagnosed inherited condition; care is handed over to us from midwives, and maintain that relationship across a network of care, until the child goes to school, where the school nurse, or SEN support will take over.
Not everyone involved has a clinical background, so for health visitors to have a heightened appreciation of genomics and the part it can play in providing equity of care, could inform multi-agency meetings, i.e. child protection conferences. It is at this type of meeting where a diagnosis can be flagged as available, which may highlight an inherited risk of certain conditions which would require preventative measures to be put in place.
The Governments ‘No Child Should be Left Behind initiative is clear, in relation to childhood vulnerability; those at risk and poor outcomes because of individual characteristics, the impact of action or inaction by other people, and their physical and social environment., as well as the child’s physical, emotional, health and educational needs. This is particularly relevant for children in care, or adopted as they are uninformed of any potential risk of developing an inherited condition, simply due to the fact of not having access to their birth family history or existing diagnosis.
With knowledge comes responsibility; there are ethical implications of genomics in public health which are complex and multifaceted. Issues such as data privacy, consent, and equitable access to genomic information need careful consideration to ensure that the benefits of genomics are distributed fairly.
Genomics has the potential to play a significant role in health visiting and public health by providing valuable insights into individual health risks, disease prevention, and targeted interventions.
Collaboration among health professionals, genetic counsellors, policymakers, and researchers is essential to successfully integrate genomics into health visiting and public health practices.
And we all need to be aware of cultural sensitivities, understanding cultural nuances in family dynamics, avoid assumptions and embrace diversity in order to support health equity for all within the population.
Nurses, midwifes and health visitors hold a very special relationship with their patient and their families. New-born screening and early intervention will support the work of colleagues within health visiting, as well as genetic counselling, education, vaccination and public health policy and planning.
https://ihv.org.uk/families/what-is-a-hv/
https://www.nhs.uk/conditions/baby/support-and-services/services-and-support-for-parents/
https://www.genomicseducation.hee.nhs.uk/genomics-in-healthcare/genomics-in-health-visiting/
https://ihv.org.uk/news-and-views/voices/understanding-genomics-new-resources-for-health-visitors/
https://ihv.org.uk/news-and-views/voices/get-ready-for-genomics-in-health-visiting/
https://www.magonlinelibrary.com/doi/abs/10.12968/johv.2022.10.7.282
https://www.genomicseducation.hee.nhs.uk/blog/hidden-genomics-in-health-visiting/
